 The Southern Illinois University Edwardsville School of Pharmacy (SOP) is partnering with the SIU School of Medicine (SOM) and SIUE School of Nursing’s (SON) regional program in Carbondale to advance the national Student Hotspotting learning collaborative.
The Southern Illinois University Edwardsville School of Pharmacy (SOP) is partnering with the SIU School of Medicine (SOM) and SIUE School of Nursing’s (SON) regional program in Carbondale to advance the national Student Hotspotting learning collaborative.
Hotspotting focuses on care coordination and follow up for “super-users,” or individuals who are admitted to the hospital multiple times a year/use the emergency department frequently, in order to reduce their need for frequent hospital/emergency visits by providing improved coordination and cost-effective medical care.
The learning collaborative is beneficial for not only patients, but also students’ leadership development, and it provides an authentic experience with interprofessional practice, says Janice Frueh, PharmD, SOP clinical associate professor in the Department of Pharmacy Practice and SOM adjunct assistant professor in the Department of Family and Community Medicine.
“Student Hotspotting’s main goals are to develop students’ abilities in working with medically and socially complex patients by gaining experience in addressing patients’ barriers to care, identifying the importance of patient-centered coordinated care, working with interprofessional teams in a community learning lab versus a healthcare system environment, and developing skills utilizing data that can be applied to healthcare delivery and design,” Frueh explained.
“Navigating the healthcare system can be challenging, and the patients our students are working with have complex healthcare needs,” said Melodie Rowbotham, PhD, RN, CNE, and director of the SIUE regional nursing program. “By developing trusting relationships with patients, nursing students can then advocate to ensure these patients receive the care they need to improve their healthcare outcomes.”
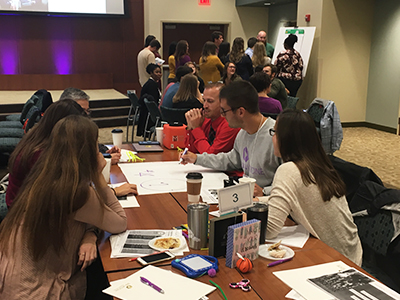
The six-month learning collaborative hosted a September kickoff event in Springfield, where interprofessional team members gained an overview of the Student Hotspotting curriculum, and explored challenges and opportunities with regard to patient engagement that the team may encounter.
“Student Hotspotting was developed from the work of the Camden Coalition in Camden, New Jersey,” said Frueh. “Its educational design follows an emerging area of medical education called Value-Added Education, that focuses on developing experiential, interprofessional education in which students provide ‘value’ to the healthcare system. Most importantly, students are to serve roles in which they interact with patients on a firsthand basis.”
The SOM has been a Student Hotspotting hub since September 2017. It is one of four institutions in the country serving as a regional learning center for other schools/teams.
“Through Camden’s partnership and guidance, hotspotting has allowed us to improve access to care for those who are struggling to achieve health in our current healthcare system,” said Tracey Smith, DNP, Student Hotspotting program lead, and research associate professor and director of population health integration at the SOM. “Using hotspotting techniques, we are helping individuals and families gain independence from the emergency room and achieve a better quality of life.”
“The greatest reward comes when individuals and families trust us enough to allow us to assist them when they are sick,” Smith said. “I hope that this program allows healthcare learners to experience that feeling of reward that so often is missing from healthcare practice.”
Faculty have found the learning collaborative to be an effective way to connect and build relationships with other educators, practitioners and researchers.
“Faculty from these institutions are building deeper relationships and collaborative work opportunities with each other,” Frueh said. “We haven’t even scratched the surface on all the possibilities related to these institutions’ curriculum, community outreach and/or strategic plans.”
Photo: Students from SIUE Schools of Pharmacy and Nursing were among those attending the Student Hotspotting learning collaborative event held in Springfield in September.